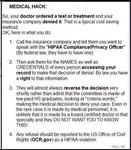
health insurance advice for what to do if your insurance deems a treatment 'not medically necessary' from Denise dreamwidth thank you Denise Digital Discipline
Digital Discipline
 Digital Discipline
Digital Discipline
a pillar of the internet as always
oh this is so good
oooooh

lolol
I will add as someone who used to write these professionally, always know your appeal rights. You should always have at least two formal written appeals where you can raise any issues on an official record. Insurance is expecting a lot of their algorithm-based decisions to just roll through because people don't know they can appeal.
There should always be appeal instructions in any denial letter you receive. They should also always be included somewhere in your master plan document-the big one that nobody reads all the way through. If they aren't, they are in violation.
These are usually reviewed by doctors, but not always. Do keep in mind that appeals do not always work, but if you intend on going legal, you'll need proof that you've exhausted the appeals process, and that you pointed out any issues and the insurance company ignored them.
Takes down notes...
I wonder if this also works for things categorically deemed 'cosmetic' that are, in a significant number of cases, actually necessary for quality of life...
Thank you for this.
SheElf You need to see this and read both linked things. This could be very useful for us both
As a Healthcare professional, yeah the auto denial nonsense is a basic filter to just make people give up through annoyance or appeal to authority ("Well they said so"). But unless it's an auto insurance or workers comp deal insurance will usually cave on the first sign of pushback
Lots of times because every time they put up a fight and prolong the process someone gets worse and that can be documented and brought to court and then alllll the bills are on them. You'll still get some stupid ass "no you can't get an mri until you have PT" despite the fact the mri can guide therapy, but don't get me started
 Break The Chains⚡️ (@bdubcali.bsky.social)
Break The Chains⚡️ (@bdubcali.bsky.social)